Fast Health: Tampered Healthcare Costs By Managing Reversing Diabetes
In the U.S., obesity and diabetes have been on the rise for generations. The health complications and long-term consequences have reverberated throughout the culture as diet fads have been pushed via the media and their efficacy touted only to be replaced by a new diet the following year.
So far, the approach by the Centers for Disease Control (CDC) in the battle against diabetes has been to educate on risk factors and preventive practices that could save people from the pain of this life-long disease. The statistics posted by the CDC have all pointed toward a common denominator: obesity. The CDC found that people with prediabetes could “cut [their] risk of getting type 2 diabetes in half” by “eating healthy and being more active.”
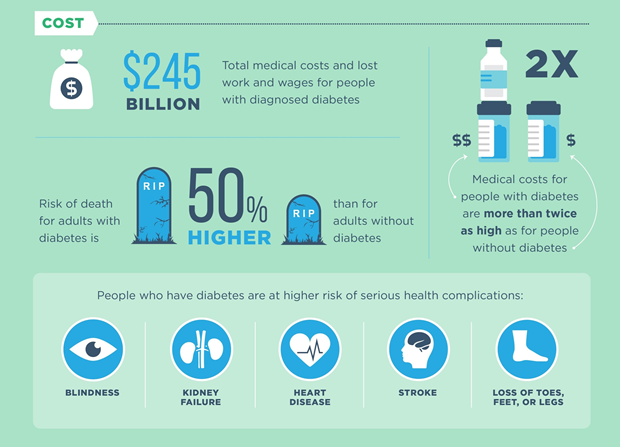
Source: CDC
Regardless of which diet has been in vogue, the rate of obesity has continued to increase. A 2012 study published in the American Journal of Preventive Medicine forecasted “a 33% increase in obesity prevalence and a 130% increase in severe obesity prevalence over the next 2 decades.” The same study estimated that “if obesity [remained] at 2010 levels, the combined savings in medical expenditures over the next 2 decades would [have been] $549.5 billion.”
The 2018 National Diabetes Statistics Report published by the CDC revealed
“… the total direct and indirect estimated cost of diagnosed diabetes in the United States in 2012 was $245 billion…. After adjusting for age group and sex, average medical expenditures among people with diagnosed diabetes were about 2.3 times higher than expenditures for people without diabetes.”

People with diabetes were found to have a greater risk of health complications such as blindness, heart disease, kidney failure, stroke, and loss of toes, feet, or legs. In 2015, “diabetes was the seventh leading cause of death in the United States.”
Combating Rising Healthcare Costs
The national average employers have been paying for type 2 diabetic employees has been an additional $10,000 PMPY, not including comorbidities or lost productivity. Employers have been throwing more drugs and money at this problem for decades, and it has not moved the needle.

The drugs prescribed for diabetes were never intended to reverse diabetes; they were intended to slow the progression of the disease. There has not yet been a drug capable of reversing diabetes, which means that treating type 2 diabetes with insulin is like treating alcoholism with more alcohol.
Increasingly, employers in the U.S. have been combating rising healthcare costs by investing in accessible preventive healthcare and education on health and nutrition for employees. This has proven to be a win-win situation. Employers have saved money, and employees have enjoyed better health and quality of life.
The Fasting Method
Dr. Jason Fung, MD, a Canadian nephrologist and author of The Diabetes Code, asserted that there has been a way to reverse type 2 diabetes without drugs or surgery. With intermittent fasting, patients were able to phase out insulin in as little as two weeks. Backed by evidence-based science and Dr. Fung’s clinical experience, The Fasting Method was designed to provide resources to help people regulate energy intake and reap the benefits of weight loss, lowered insulin levels, and autophagy.
Totem recognized the concern of employers who have doubted their ability to engage employees in a program like the Fasting Method, even if they could identify all of their diabetic and pre-diabetic employees. Due to this concern, Totem partnered with Dr. Jason Fung and his team to deliver his clinical approach to employers across the country.
In creating the program, Dr. Fung’s team took into consideration that fasting may be an unknown paradigm for participants. The program was constructed to teach employees about fasting, connect them with a fasting coach 2-4x per month, and then report on the participation and outcomes so companies could see a real ROI.
Alternatively, employers who have continued to double down on diabetes “management” have not made a dent in their diabetes spend, and their employees have become sicker in the process.

Weight loss was not the only benefit of intermittent fasting.
Those who have adopted intermittent fasting (IF) have discovered an inherent caloric restriction in the practice. As they became more thoughtful of what they ate and when they ate, many of the added calories from late night eating vanished. However, if caloric restriction was the only benefit of IF, then caloric restriction could have been applied without restricting eating windows.
Presently, many IF studies have been conducted on animals, making the findings subject to skepticism, but even though there have been a scarce number of IF studies conducted on humans, the evidence substantiated by human studies has been sufficient to turn heads. In one of these IF studies conducted on humans, researchers from the University of Alabama observed a group of eight obese pre-diabetic men on early-time restricted feeding compared to twelve hour restricted feeding.
Researchers noted that in previous studies of time restricted feeding (TRF) trials, the specific time of day of the eating window affected results. They noticed that the body’s internal biological clock, known as the circadian system, was having an impact on the data, indicating “that combining two different meal timing strategies—IF and eating in alignment with circadian rhythms—may be a particularly beneficial form of IF.” Data taken from human TRF trials suggested that food intake in the morning was optimal for the human metabolism when insulin sensitivity and food digestibility were higher.
During the randomized controlled trial (RCT), the group of men had a daily eating window of six hours with dinner before 3pm for five weeks. In an effort to test the effectiveness of IF without the weight loss factor, there was no caloric deficit or surplus. Participants were given enough food to maintain their weight and only received food by the study staff, making it the most controlled RCT conducted on humans for the study of IF to date.
In seven out of eight participants, insulin sensitivity improved, insulin levels were lowered, and blood pressure was lowered without any weight loss. Intermittent fasting proved to have health benefits beyond weight loss.
Autophagy was activated by fasting.
Studies have shown that one of the greatest benefits of fasting is autophagy, which could be described as cellular cleansing. The literal translation of the latin-derived word is self-eating. Autophagy occurs when the deteriorated organelles of the cells are discarded and metabolized. The damaged organelles become fuel for regenerating new and healthier cells.
Autophagy is engaged only in a fasted state of at least twelve hours and continues until food is consumed, at which point, the body shifts gears into metabolizing the incoming nutrition. Autophagy can never be activated while the digestive organs are burdened with food.
The 2014 study, Fasting: Molecular Mechanisms and Clinical Applications, analyzed the major factors that have afflicted overweight people of overfed and sedentary generations by looking at the data of 112 studies. Among elevated glucose, insulin, and inflammation, the “accumulation of dysfunctional proteins and organelles” was also a recurring factor. Based on the body of evidence dissected, the study concluded that periodic fasting could be optimum for adult health, reducing the risk of chronic diseases and promoting anti-aging due in part to the effects of autophagy.
Ultimately, the combination of weight loss, reduced insulin levels, and the activation of autophagy have made intermittent fasting one of the most advantageous preventive health tools known to man.
References
Finkelstein, E. A., Khavjou, O. A., Thompson, H., Trogdon, J. G., Pan, L., Sherry, B., & Dietz, W. (2012). Obesity and Severe Obesity Forecasts Through 2030. American Journal of Preventive Medicine, 42(6), 563–570. doi: 10.1016/j.amepre.2011.10.026. https://www.ajpmonline.org/action/showPdf?pii=S0749-3797%2812%2900146-8
Furmli, S., Elmasry, R., Ramos, M., & Fung, J. (2018, September 18). Therapeutic use of intermittent fasting for people with type 2 diabetes as an alternative to insulin. Retrieved from https://casereports.bmj.com/content/casereports/2018/bcr-2017-221854.full.pdf
Longo, V. D., & Mattson, M. P. (2014, February 4). Fasting: molecular mechanisms and clinical applications. Retrieved from https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3946160/pdf/nihms551820.pdf
National Diabetes Statistics Report. (2018, February 24). Retrieved from https://www.cdc.gov/diabetes/pdfs/data/statistics/national-diabetes-statistics-report.pdf
Sutton, E. F., Beyl, R., Early, K. S., Cefalu, W. T., Ravussin, E., & Peterson, C. M. (2018). Early Time-Restricted Feeding Improves Insulin Sensitivity, Blood Pressure, and Oxidative Stress Even without Weight Loss in Men with Prediabetes. Cell Metabolism, 27(6), 1212–1221. doi: 10.1016/j.cmet.2018.04.010. https://doi.org/10.1016/j.cmet.2018.04.010 The Science. (2020, January 6). Retrieved from https://thefastingmethod.com/the-science/




