According to the CDC, by June 2020, 41% of the U.S. had delayed or avoided medical care including both routine and urgent or emergent care. Delay and avoidance of medical care may increase the mortality risks for treatable and preventable health conditions. This could also in turn contribute to inflated reported COVID-19 death statistics.
Employers are encouraged to understand why employees are delaying and avoiding healthcare and provide targeted education and communication to encourage safe, timely routine and urgent care. This CDC article describes more about the delay of healthcare due to COVID and which demographics have been highly impacted.
U.S. Employers Experiencing Lower Health Benefit Costs in 2020
Care avoidance and delay has done what no pandemic has ever done in history: it has lowered healthcare costs compared to 2020 projections. Experts estimate that 2020 costs will be between 3% and 9% lower than expected, which is a significant savings for employers. Although this is good news for employers in the short run, COVID-19’s deferred treatments and long term impact on health care is uncertain.

What can we expect in 2021?
Although the extent of continued care avoidance is unknown, in 2021, overall costs are expected to rise again by between 4% and 10%, according to PwC. This is primarily due to continued care for COVID-19 patients and delivery of previously deferred care. Care avoidance and delay will also be impacted by the vaccine distribution timeline. Additionally, due to the uncertainty of COVID, most employers are not increasing costs for employees for 2021 – in fact, according to a Mercer survey, 57% of employers are not increasing deductibles and copays for 2021.
What can employers do to minimize care avoidance and delay?
Virtual care using phone and video has allowed physicians to continue treating patients while following social distancing recommendations.
As the pandemic continues, the comfort level with and popularity of virtual visits is expected to continue to increase. The pandemic has proven that both physicians and patients have embraced virtual care, and much of this is likely here to stay. This will reduce the cost per episode and have favorable impacts on health care costs.
80% of large employers believe telehealth will play a significant role in the delivery of healthcare in the future. Over 90% of large employers plan to expand virtual care to include mental health, and 54% plan to waive those costs for employees in 2021.
Not all Virtual Care is the Same
To ensure employees receive continued care during the pandemic, a distinction should be made between telemedicine and virtual direct primary care. Telemedicine manages non-complex conditions and illnesses and provides convenient access to a licensed physician for quick assistance. Physicians can diagnose, treat, and issue prescriptions, and the patient is able speak to any of the various physicians in the telemedicine “network” at the time of needed care.
Virtual Primary Care Physician / Patient Relationship and Scope of Treatment
Virtual direct primary care (DPC) facilitates a physician and patient relationship that doesn’t t exist with telemedicine. Employees have access to their primary care doctor (the same physician) on a continuous basis for all healthcare needs. The physician is able to manage the patient as a whole without the time constraints of office visits.
In addition to treating acute care needs such as respiratory conditions, viral/bacterial infections, flu., colds, minor injuries, virtual direct primary care physicians help patients manage chronic conditions (i.e. diabetes, allergies, asthma, high blood pressure). Preventive care services are also provided, with referrals to labs as appropriate. The need for mental health services is on the rise as a result of the pandemic, and most direct primary care vendors include mental health services. Studies show that online mental health therapy is as effective as the traditional model, primarily because the online model relieves some anxiety of discussing mental health concerns.
Virtual Primary Care Physician Access and Cost
Typically, the cost for virtual primary care is a per employee per month fee that includes unlimited access to the physician care team. Fees for employer-paid programs typically range from $15 to $40 PEPM, depending on the size of the group and vendor. The program can also be offered on an employee-paid basis, and many employers view this benefit as a great retention tool.
Employees have 24/7 access to the physician team for ongoing needs and concerns with typical response times ranging between 7-15 minutes. This model is tremendously efficient because the traditional model requires a physical appointment regardless of the concern, a simple question or a more complex medical need. Patients can easily communicate with physicians about concerns and questions through the app or by phone.
Direct primary care can avoid up to 90% of specialist visits, but the direct primary care team is able to refer to participating network specialists as appropriate. This model saves the employer 5 to 10% of total healthcare costs, allowing employees unlimited access for a minimal monthly fee without a per visit or office visit copay.
Direct primary care programs provide tremendous value for both patients and employees. According a Nextera Healthcare case study, results show a 41% reduction in urgent care visits, 10% reduction in ER visits, 92% fewer inpatient admissions, and 77% less outpatient hospital visits when comparing DPC members to non DPC members.
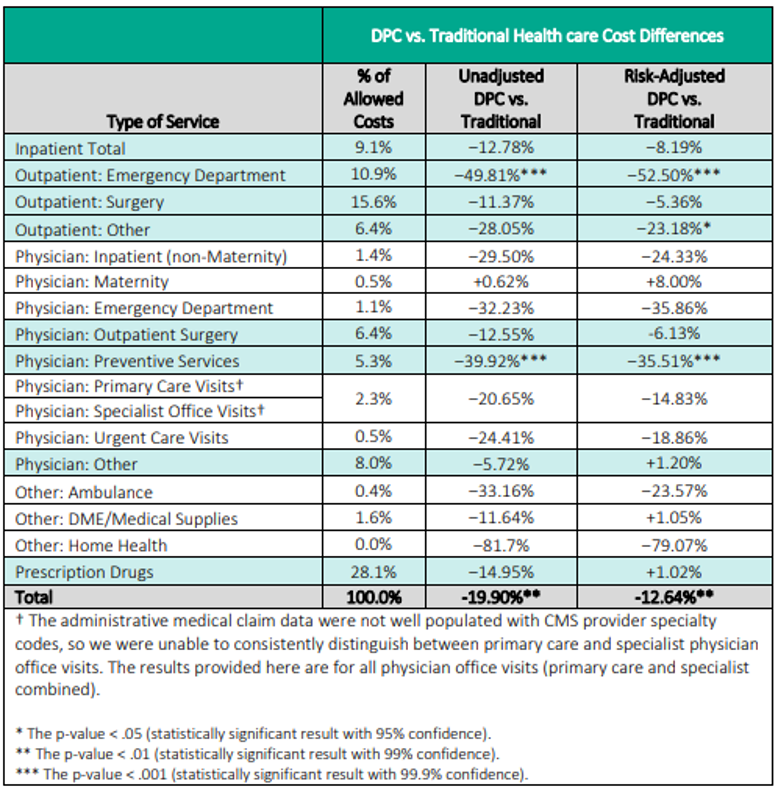
Lastly, the Milliman study results show an overall cost savings of 13% when comparing DPC to traditional healthcare models.